Abstract
Background: Despite advances in novel myeloma treatments and autologous hematopoietic stem cell transplantation (ASCT), allogeneic HSCT (alloSCT) remains the only curative option for patients (pts) with multiple myeloma (MM). Questions remain as to the timing of alloSCT, toxicity risks and optimal conditioning regimen. The addition of bortezomib (Vel) to fludarabine (Flu) and melphalan (Mel) for conditioning prior to alloSCT is based on the demonstrated safety of Vel in combination with melphalan prior to ASCT, the synergistic effect of Vel with Mel, and the ability of Vel to selectively eliminate allo-reactive T-cells.
Methods: We present a prospective Phase II study using Flu/Mel/Vel (FMV) as a conditioning regimen for alloSCT. The primary endpoint is overall survival (OS), and secondary endpoints include progression free survival (PFS), incidence of graft-versus-host disease (GVHD) and transplant related mortality (TRM). For related donors, the conditioning regimen was Flu 30 mg/m2 days -5, -4, -3, -2, Vel 1.6 mg/m2 days -4, -1, Mel 140 mg/m2 day -2. For unrelated donors, rabbit ATG 4 mg/kg was given in divided doses days -3, -2, -1. GVHD prophylaxis consisted of methotrexate and tacrolimus. We compared pts receiving FMV to historical controls of pts receiving FM at the same dose and schedule without Vel. We also compared pts receiving FMV to all pts with MM treated with alloSCT including all regimens and donor types.
The response criteria from the IMWG and M-Smart criteria were used to determine response and risk, respectively. Chi-square tests of association and Wilcoxon rank sum tests were performed to test for differences across groups. OS/PFS probabilities were calculated using the Kaplan-Meier product limit estimator with log rank-tests. Multivariate Cox proportional hazard models examined factors associated with OS/PFS.
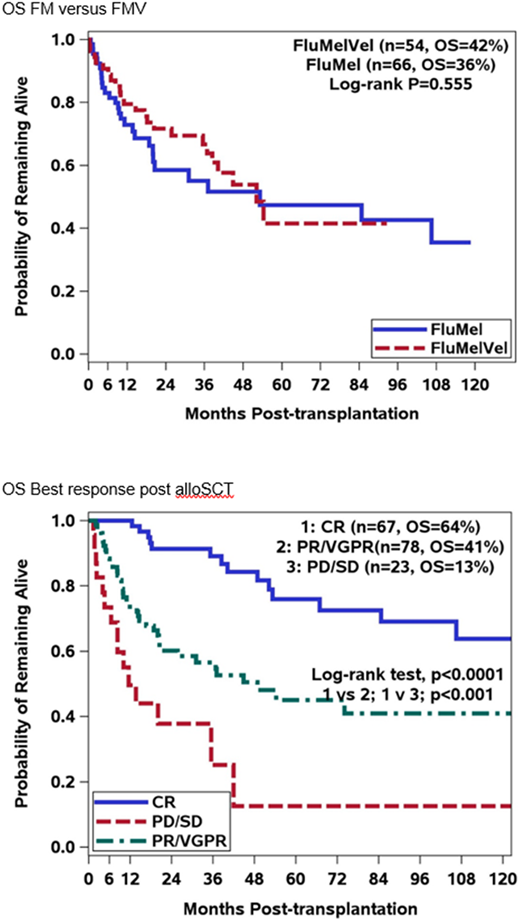
Results: Of the 54 pts who received FMV, 35 (65%) were male and the median age was 56 years. Twenty-seven pts had an HLA matched sibling donor and 27 had an unrelated donor. At the time of alloSCT, 5 pts were in a CR, 27 in a VGPR, 13 in a PR, 9 had < PR. Twenty eight pts (52%) had high risk disease. Twenty-nine pts (53%) received alloSCT as salvage, defined as relapsed or refractory to ASCT, and 25 pts (46%) as consolidation after ASCT. OS was 42% at 10 years. While 32 pts developed aGVHD, only 2 had ≥ Grade 3. Of the 31 pts who developed cGVHD, 23 were graded as extensive. TRM was 5% at day 100, and 15% over 10 years.
Pts in the control groups had similar baseline characteristics to the FMV group. The only significant difference was 47 pts (72%) who received FM were transplanted as salvage, and 18 (28%) as consolidation after ASCT (p=0.035). The total number of pts who did not receive FMV (non FMV) was 121, with 66 pts receiving FM. Compared to pts who received FMV, there was no difference in OS for pts who received FM or the non FMV group, 35% (p=0.55) and 48% (p=0.855) respectively. There was no difference in pts who developed aGVHD, however 9 pts (13%) had ≥ grade 3 aGVHD in the FM group (p=0.004) and 15 (12%) in the non FMV group (p=0.006). The cumulative incidence of cGVHD was similar with 51% for pts receiving FM and 60% for FMV pts (p=0.32). TRM was similar to pts who had received FMV; 18% for FM and 17% for non FMV. There were no differences between the 3 groups across disease risk, donor type, or disease status at the time of alloSCT. Multivariate analysis of the 3 groups, shows achieving a CR after alloSCT (p=0.0006) or having cGVHD (p=0.0004) predicts for improved OS, while severe aGVHD (p=0.0002) predicts for decreased OS.
Discussion: While FMV was associated with a lower incidence of severe aGVHD, the addition of bortezomib to the FM backbone did not improve PFS or OS. Day 100 TRM was low for all regimens, and the addition of Vel did not impact overall TRM. For all 175 pts, those who achieve a CR after alloSCT had a significantly improved OS. This prompts the question of whether strategies should be employed post alloSCT to maximize response to a CR, and the role of achieving MRD negativity after alloSCT also needs to be elucidated.
Siegel:BMS: Consultancy, Honoraria, Speakers Bureau; Novartis: Honoraria, Speakers Bureau; Celgene: Consultancy, Honoraria, Research Funding, Speakers Bureau; Merck: Consultancy, Honoraria, Speakers Bureau; Janssen: Consultancy, Honoraria, Speakers Bureau; Karyopharm: Consultancy, Honoraria; Takeda: Consultancy, Honoraria, Speakers Bureau; Amgen: Consultancy, Honoraria, Speakers Bureau. Biran:Amgen: Consultancy, Speakers Bureau; BMS: Research Funding; Merck: Research Funding; Takeda: Consultancy, Speakers Bureau; Celgene: Consultancy, Honoraria, Speakers Bureau. Skarbnik:Jazz Pharmaceuticals: Honoraria, Speakers Bureau; Pharmacyclics: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Genentech: Honoraria, Speakers Bureau; Seattle Genetics: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Honoraria, Speakers Bureau; Gilead Sciences: Honoraria, Speakers Bureau; Abbvie: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.